Last updated: November 16, 2018
Before you can submit a claim online, you have to
sign up for direct
deposit and add the provider for your healthcare service or product to your account. If the provider is
already in your list, make sure their information is up to date or your claim could be denied.
Before you begin
- Check to see if your provider has been delisted before you pay for a product or service that is covered
under your plan. To view delisted providers, log in to your group insurance account, click the
Tools and resources tab and consult the
Resource Centre.
- If there’s any information you can’t see or make changes to, contact the person responsible for your
group insurance plan.
-
-
Log on to the plan member site.
Need
help to register?
From the home page, select
Submit a claim > Online claim.
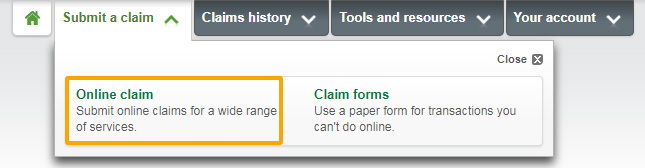
Don’t see this option?
That means online claims aren’t available for your plan. Select
Submit a claim > Claim forms instead to find forms pre-filled
with your plan information.
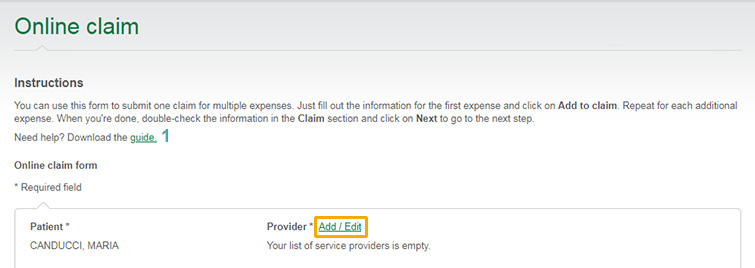
In the online claim form, click
Add/Edit next to the
Provider field.
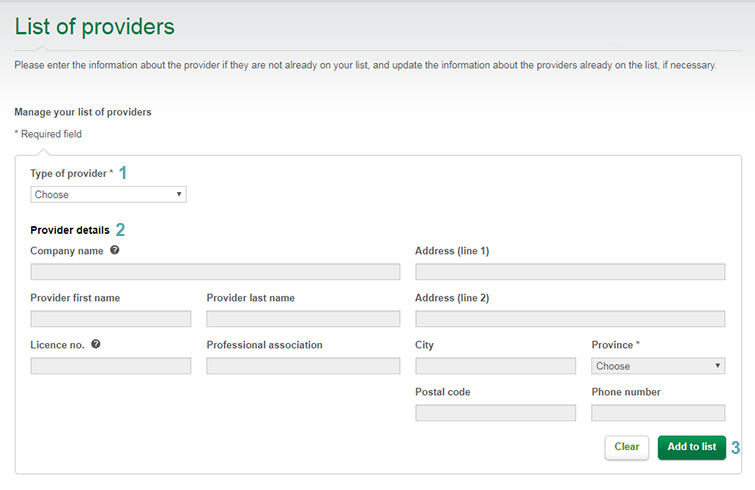
In the
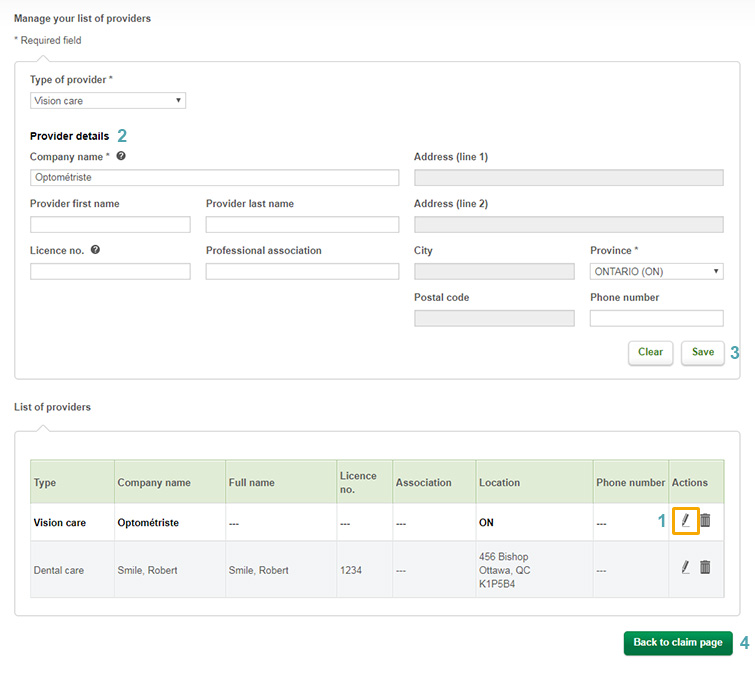
Type of provider drop-down list
(see 1 in the List of providers screenshot), select the
option that matches your claim.
Can’t find your healthcare provider in the drop-down list?
That means you’ll have to fill out a paper form and mail it to us. From the home
page, choose
Submit a claim > Claim forms to find forms pre-filled with your
plan information.
Complete all the required fields marked with an asterisk (*)
(2) and click
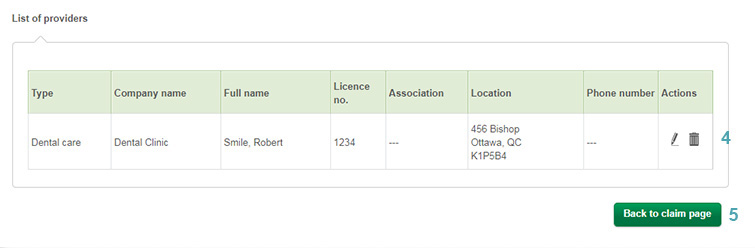
Add to list(3). The provider should now
appear on your list
(4). To submit your online claim, click
Back to claim page(5).
Good to know!
If you update your provider list from the plan member site, the changes will
automatically appear in the Omni app, and vice-versa!
Scroll down to the
List of providers at the bottom of the page and find the one you want to
edit. Click the
pencil icon in the right-hand column
(see 1 in the Manage your list of providers screenshot).
This will open up that provider’s information at the top of the screen
(2). Make the changes you need to make and click
Save(3). To submit a claim, click
Back to claim page(4).
If you want to delete a provider from your list, click the
trash can icon next to their name. A pop-up message will ask you to
confirm. Click
Yes.
Good to know!
When you update your provider list from the plan member site, the changes will
automatically be made in the Omni app, and vice-versa!